The potential for improving cardio-renal outcomes in chronic kidney disease with the aldosterone synthase inhibitor vicadrostat (BI 690517): a rationale for the EASi-KIDNEY trial
Nutritional information
What You Need to Know

Anaemia
Anaemia, characterised by a decrease in the number of red blood cells, is very frequent in haemodialysis.
Anaemia is already present before dialysis because it is essentially linked to a deficit in erythropoietin (EPO), a hormone produced by the kidneys that stimulates the production of red blood cells by the bone marrow.
When haemoglobin levels drop under 10g%, your nephrologist will usually propose an EPO treatment.
A healthy diet and sufficient physical activity are associated with a better control of anaemia. Iron deficiency is common mainly due to a decrease in absorption. Sometimes oral supplementation is necessary. A sufficient intake of Vitamin C found in fruit and vegetables promotes iron absorption. A decrease in Vitamins B1, B6, B9 and B12 in relation to a restricted diet and malnutrition could be avoided with a well-balanced diet. Your dietician will be able to help you choose adequate nutrients.
Sometimes vitamin supplements are necessary.
Philippe Chauveau, France
Calcium, phosphorus and bone
The kidney is an important organ for bone metabolism. Kidney diseases cause high levels of phosphate, parathyroid hormone (PTH) and low levels of calcium and Vitamin D. These problems occur in the early stages of chronic kidney disease (CKD), most of the time without clinical symptoms. Later, during the course of CKD, bone disease worsens and extra-vascular calcifications, bone pain or an increased risk of fracture could occur.
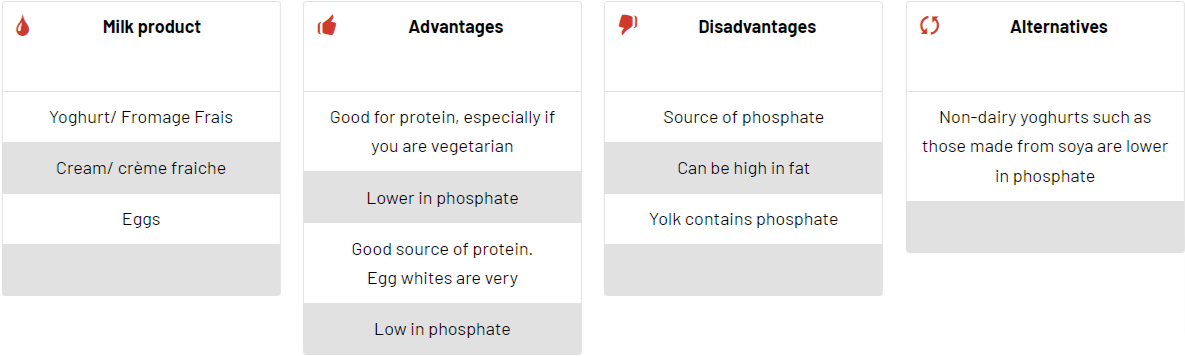
Patients should decrease phosphorus intake and avoid foods with higher phosphorus content. Fish, meat and eggs contain phosphate, but should not be decreased without a nephrologists’ advice because of their nutritional value. Most of the time phosphate content in nutrients is hidden and you need dietician advice to choose low-phosphate nutrients and cooking instructions.
This cookbook will help you to choose low phosphate content and high nutritional value foods.
Calcium intake should be normal.
Vitamin D supplementation is usually prescribed. Specific medication for hyperparathyroidism exists in case of very high levels of PTH.
Phosphate binders help to lower blood phosphate levels. Many types of this medication exist. Your doctors will explain to you and prescribe the type of phosphate binder recommended for your personal case.
Philippe Chauveau, France
Cheese, dairy, dairy free alternatives and eggs

Cheese and phosphate content
Lina Johansson, United Kingdom
Diabetes in haemodialysis patients
Good control of diabetes in haemodialysis is essential to prevent long-term complications including damage to the heart, vessels and eyes. Whether diabetes requires insulin or not (insulin-dependent diabetes or “mature” diabetes), the diet must be personalised and adapted to haemodialysis. Only blood glucose levels are useful for follow-up. The determination of glycosylated haemoglobin (HbA1c) depends upon the control of diabetes over a longer period.
The basic prescription for insulin-dependent diabetes is similar to that of the prescribed level before dialysis: 35 kilocalories per day, 50% of which is in the form of carbohydrates. In order to avoid hyper- and hypoglycaemia, the distribution during the day often consists of 3 meals and 2 snacks.
The most important thing is that the diet must be established with a dietitian and regularly reviewed, taking into consideration the different types of sugars (slowly digested or fast ones, little or a lot of hyperglycaemic).
Maintaining a good level of physical activity is very important.
An adequate intake of fruit and vegetables must be maintained. Avoid a high intake when potassium levels are too high (see the section on potassium).
Snacks should be adapted to dialysis sessions. The bath usually contains one gram of glucose, but hypoglycaemia can still occur.
Christoph Wanner, Germany
Energy intake
Non-dialysed patients with advanced chronic kidney disease and those undergoing maintenance haemodialysis or chronic peritoneal dialysis should be prescribed a dietary energy intake of 35 kcal/kg/day for patients who are <60 years of age and 30 kcal/kg for patients ≥60 years of age (1,2,3). Overweight or undernourished patients may need adjustments of energy supply. Carbohydrates equate to 50-60% of daily total energy intake and fat should account for 30-40%. Carbohydrates from sugars should be limited to less than 10% of energy intake, and higher polyunsaturated and monounsaturated fat consumption rather than saturated fatty acids, trans-fat and cholesterol are associated with more favourable outcomes (4). The KDIGO Clinical Practice Guidelines for Diabetes and CKD recommends that 40-45% of calories from carbohydrates should come from whole grains, fruit and vegetables [5] and the Kidney Disease Outcomes Quality Initiative (KDOQI)’s ‘Guidelines on Dyslipidemia’ recommends 20–30g/day of fibre [6]. Patients treated with peritoneal dialysis absorb calories from the glucose in the dialysis fluid and this should be included in the calculation of dietary energy intake. Approximately 90% of the glucose is absorbed during dwells over 8h, and about 70% is absorbed during shorter dwells; therefore, the amount of carbohydrate absorbed in each exchange can be estimated (7). Replacing saturated with polyunsaturated fats may modulate hyperlipidaemia. In patients with hypercholesterolaemia, a diet including ≤30% of energy as fat, 10% saturated fatty acids and less than 300mg/day dietary cholesterol intake is recommended (8).
Resting energy expenditure (REE) is normal in stable maintenance chronic kidney disease and dialysis patients. During haemodialysis, studies have found an increase of 12-20% in the presence of co-morbidities, severe hyperparathyroidism, inflammation and poorly controlled diabetes (9,10,11,12). Decreased physical activity, leading to a reduction rather than an increase in total energy expenditure might have mitigated the increased REE (13).
Siren Sezer, Turkey
References
- Clinical Practice guidelines for nutrition in chronic renal failure.K/DOQI, National Kidney Foundation. Am J Kidney Disease 2000;35:S1-140
- Fouque D, Vennegoor M, ter Wee P et al. EBPG guidelines on nutrition. Nephrol Dial Transplant 2007;22 suppl 2:45-87
- Toigo G, Aparicio M, Attman PO,et al. Expert working group report on nutrition adult patients with renal insufficiency (part 2 of 2). Clin Nutr 2000;19:281-291
- Gang JK, Kalantar-Zadeh K, Goldstein-Fuchs J, Rhee CM. Review Dietary Approaches in the Management of Diabetic Patients with Kidney Disease.Nutrients 2017, 9, 824. doi:10.3390/nu9080824
- National Kidney Foundation (2007) KDOQI™ clinical practice guidelines and clinical practice recommendations for diabetes and chronic kidney disease. Am J Kidney Dis 49(suppl 2):S1–S180
- Kidney Disease: Improving Global Outcomes (KDIGO) Lipid Work Group (2013) KDIGO clinical practice guideline for lipid management in chronic kidney disease. Kidney Int Suppl 3:259–305
- Wolfson M. Management of Protein and Energy Intake in Dialysis Patients J Am Soc Nephrol 1999;10: 2244–2247
- Toigo G, Aparicio M, Attman P-O etal (2000) (ESPEN) Expert Working Group report on nutrition in adult patients with renal insufficiency (part 1 of 2). Clin Nutr 19:197–207
- Neyra R, Chen KY, Sun M, Shyr Y, Hakim RM, Ikizler TA. Increased resting energy expenditure in patients with end-stage renal disease. JPEN J Parenter Enteral Nutr. 2003;27:36-42.
- Cuppari L, de Carvalho AB, Avesani CM, Kamimura MA, Dos Santos Lobao RR, Draibe SA. Increased resting energy expenditure in hemodialysis patients with severe hyperparathyroidism. J Am Soc Nephrol. 2004;15: 2933-2939.
- Avesani CM, Cuppari L, Silva AC, Sigulem DM, Cendoroglo M, Sesso R, et al. Resting energy expenditure in pre-dialysis diabetic patients. Nephrol Dial Transpl. 2001;16:556-565.
- Utaka S, Avesani CM, Draibe SA, Kamimura MA, Andreoni S, Cuppari L. Inflammation is associated with increased energy expenditure in patients with chronic kidney disease. Am J Clin Nutr. 2005;82: 801-805.
- Avesani CM, Trolonge S, Deleaval P, Baria F, Mafra D, FaxenIrving G, et al. Physical activity and energy expenditure in haemodialysis patients: an international survey. Nephrol Dial Transpl. 2012;27:2430- 2434.
Fish
Fish and meat are very rich in proteins of high biological value (essential for the body).
Fish is poor in connective tissue and fat. It is digested faster than meat. The carbohydrate content is low.
Fish contains high-quality protein with all the essential amino acids, whose use should be optimised. This is particularly useful in case of a reduction in protein intake.
Fish could be classified according to its fat content however, you should know that fattier fish contain less fat than the least fatty meat!
Some fish contain certain polyunsaturated lipids (omega-3) that fight against atheroma and reduce cardiovascular disease. Fish highest in omega-3 fatty acids include albacore tuna, herring, mackerel, rainbow trout and salmon.
Fish can be consumed instead of meat in the same quantities at least twice a week.
Fish can be cooked in many different ways associated with different vegetables and starchy foods, which makes it attractive and allows you to vary the weekly menu.
How much fish (or generally seafood) you can eat depends on your CKD stage. Nutrient content varies. Some are rich in potassium, phosphorus or salt. Your dietician can help you in your choice.
Philippe Chauveau, France
Fluids
In the early stages of kidney disease, it is not necessary to limit fluid intake.
If your kidney disease gets worse, your dietician or nephrologist will advise you on the amount of fluids to consume each day.
Reducing liquid consumption may be difficult for haemodialysis patients when it is recommended to increase this in end-stage renal failure. Due to the decrease in diuresis (amount of urine produced), water (and waste) is accumulated. It is therefore essential to remove the excess to avoid fluid overload causing fatigue to the heart. Reducing the consumption of liquids limits weight gain between dialysis sessions. Excessive weight gain between sessions can lead to a drop in blood pressure and significant fatigue after dialysis.
What are the recommendations?
They concern all fluids and not just water.
In case of diuresis: equivalent in volume to your diuresis plus 500 to 750ml of fluid.
In case of anuria: 500 to 750ml of fluids per day.
We tend to overestimate the water intake of food and wrongly stigmatise certain foods because of the specific juices it releases.
Overall, a day of food consumption (not counting the intake of liquids) equates to 1L of water.
Stanislas Trolonge, France
Beverages concerned
- Tea, coffee, chicory
- Milk
- Juice
- Still or sparkling water
- Soups and broths
- Sugary drinks
- Alcohol
Tips to limit your liquid consumption
- Use smaller containers: a small cup instead of a larger one to reduce the amount of liquid consumed.
- To quench your thirst, suck ice cubes or frosted orange or lemon slices. Thus, you limit the intake of liquids.
- Some tablets or powders that need to be diluted can be swallowed with food, which avoids an additional intake of liquids.
- During hot weather, drink cool beverages or use a fan to cool off.
- Avoid overheated rooms. You can humidify the surrounding air by placing a water container on the radiator.
- Alcoholic or sweet drinks do not quench your thirst; they will make you even thirstier.
- As an aperitif, avoid drinks that require adding water (e.g. aniseed aperitif …).
Fruit and Vegetables
Fruit and vegetables are essential for health as they provide a range of vitamins and minerals as well as being an excellent source of fibre. They are also low in fat.
There are concerns that some fruit and vegetables are very high in potassium (see section on potassium). Taking this into consideration, some useful tips can be found below to help you decide which fruit and vegetables are best to consume and how to prepare them.
Fruit and vegetable juices tend to be very high in potassium and best avoided, as are soups made from vegetables.
Vegetables Cooking methods
Reducing the load of dietary potassium is recommended in case of, or to prevent, hyperkalaemia in CKD or dialysis. One of the strategies is cooking food. Fruit and vegetables are foods rich in potassium. Proper cooking methods significantly reduce the food’s potassium content once cooked.
Cooking by boiling in plenty of water lowers the potassium content of vegetables.
Double cooking is recommended for cooking vegetables, fruit and potatoes.
In practice, two saucepans of water will be boiled at the same time so as not to waste time.
Recommendation: If you peel vegetables (e.g. potatoes) before boiling, this will further increase the potassium loss.
The initial cooking of the food will take place in the first saucepan of water for 10 to 15 minutes. This cooking water should then be thrown away. The food will then be deposited in the second saucepan of boiling water to finish cooking. For additional flavour, food can be sautéed in a frying pan using fat, herbs and spices.
Ask your nephrologist or dietician for advice on the best choice of foods, recommended portions and recipes using these cooking techniques.

Nutritional tables
Lina Johansson, United Kingdom
Stanislas Trolonge, France
Herbs and spices
Herbs and spices can be used in order to give additional taste to food. For example:
- Sweet paprika or cayenne can give additional flavour to beef, poultry, seafood, soups, sauces and most vegetables.
- Celery can be added to meat, fish, poultry, soup, salads/dressings and assorted vegetables such as leeks and cabbage.
- Nutmeg provides extra flavour to creamy sauces or béchamel and in all vegetables, other than those belonging to the cabbage family.
- Mint and basil can be added to dishes with poultry, fish, meat, tomato sauces, cooked vegetables, pasta, soups and salads.
- Thyme and Oregano add flavour to poultry, fish, meat, sauces, steamed vegetables, pasta, soups, salads and grilled meats.
- Dill can be added to dishes with fish, creamy soups, potatoes, green beans, peas, spinach, carrots, eggs and lemon sauces.
- Parsley tastes good with almost all dishes, salads and sauces.
- Rosemary enhances the taste of meat (especially lamb), poultry, fish and casseroles.
- Cinnamon, allspice, bay leaves and cloves go well with almost any type of meat and especially sauces.
- Cumin can be used instead of cinnamon, although it has a more intense flavour.
- Curry and coriander can be used in oriental dishes with meat, marinades and in different fish sauces.
- Tarragon gives additional flavour to fish, asparagus, beets, cabbage, cauliflower and in marinades.
- Ginger can be added to dishes with beef, chicken, pork, green beans, cauliflower and aubergine.
Caution! Do not use salt substitutes. These products contain potassium chloride and can raise your blood potassium levels.
KalliopiAnna Poulia, Greece
Hypertension
High blood pressure (hypertension) is common during kidney failure and also in haemodialysis. It can be the cause or the consequence of the destruction of the kidneys. It is always aggravated by the excessive intake of salt and often water that accompanies it, as salt can stimulate thirst (see the section on sodium). It must be treated with drugs and a low salt diet because it is harmful to the heart and the vessels (atherosclerosis, cardiovascular diseases). In dialysis, patients with a decrease in basal weight should be discussed when arterial hypertension appears or worsens.
Adherence to medication is very important. Antihypertensive medication can occasionally cause some side effects.
Do not hesitate to discuss this with your doctor rather than modify your treatment alone.
Stanislas Trolonge, France
Lipids
Lipids come from the human diet or are synthetised by the body from sugars or alcohol. Cholesterol and triglycerides are measured in the blood. Cholesterol can be normal or high and an increase in triglycerides is common in haemodialysis patients. Both are vascular risk factors.
The fatty substances present in foods are either of animal origin (butter, pâtés, …) or vegetable origin (oils).
Fats from animal sources, with the exception of fish, contain cholesterol and saturated fatty acids that are harmful to the vessels. Vegetable fats contain polyunsaturated fatty acids protecting the vessels. Marine fats (found in fish) can be beneficial to the body.
Your lipid intake must be balanced.
It is generally necessary to reduce the intake of cholesterol by avoiding fatty meat (mutton, lamb and pork) and by opting to eat fish or lean meat (chicken, white meat) instead.
Preferably use corn and sunflower oils; limit butter to 20 grams a day for breakfast.
Christoph Wanner, Germany
Meat
The nutrient value of meat is very high. It is a food rich in high biological value proteins able to provide the full range of amino acids including essential amino acids.
It has been argued that high consumption of meat is harmful to the kidneys. In CKD, protein intake should be reduced. A reasonable consumption of meat helps to maintain the protein body store (such as eggs or fish).
White or red meat?
White and red meats have the same nutritional value.
White meats often come from young animals and their low connective tissue content makes them more digestible. However, the protein intake is almost identical:
100g of beef = 18g of protein
100g of chicken = 21g of protein
In contrast, the fat content of meat varies by species; horse being the least rich with less than 10%, the richest is duck followed by goose with 20%.
In haemodialysis, be sure to eat enough protein every day: if necessary, replace the amount of meat with its equivalent (fish or eggs) as indicated by your dietician.
For example, 100g of meat can be replaced by 100g of poultry, 100g of fish or 2 eggs.
Philippe Chauveau, France
Medication and nutrition
Kidney disease is often associated with other health problems such as diabetes, high blood pressure or heart disease. Once these diseases have been diagnosed, your doctor will prescribe an appropriate treatment plan. This could include a large number of tablets or sachets throughout the day.
Combining good nutrition, normal social life and taking treatment at the time indicated is sometimes difficult. The number of drugs can lead to forgetting something.
It is important to respect the schedules for most medications:
- Treatment against high blood pressure should usually be taken both in the morning and the evening to ensure blood tension control throughout the day and night.
- In the case of dialysis, some treatment must be taken after the dialysis session as it may subsequently be eliminated during the session.
- Phosphate binders must be taken in the middle or at the end of a meal because they bind to the phosphorus in food in the intestine to decrease its absorption.
- Some medication needs to be taken on an empty stomach, in the morning.
If you have difficulty taking the full course of treatment, or if you frequently forget certain medications, you should discuss this with someone. Your doctor, but also your nurse, pharmacist or dietician can help you.
Understanding the treatment and its usefulness is very important.
Be aware of possible side effects and feel able to talk about them, potentially leading to changing or improving the treatment.
In case of frequent forgetting, a pillbox can help you.
Habits or routines like putting the medication on the table whilst preparing breakfast may help you to remember.
It is sometimes difficult to take all medications and to understand their utility. The most important thing is to be able to talk about it with the medical staff.
Philippe Chauveau, France
Physical activity
Nowadays, everyone knows that you have to move, even just a little, and that physical activity is a real medicine. Physical activity is a weapon against chronic diseases.
However, dialysis patients are generally very sedentary (1). This sedentary lifestyle is associated with excess mortality, whereas, conversely, physical activity has many benefits in terms of physical performance, quality of life, improved sleep, reduced anxiety, asthenia (2) and mortality reduction (3).
There are many obstacles related to practising physical activity, the time already spent on dialysis (12 hours per week excluding transport) is one of the main complaints received from patients (4). However, asthenia, chronic deconditioning, and from a clinical perspective, lack of means and/or competent staff are also contributing factors
In the case of patients with chronic kidney disease, physical activity must be supervised, at least initially, by a physical activity professional. He/she will be able to make a complete evaluation in order to establish the most suitable “prescription” of physical activity for each patient.
There are many ways to increase physical activity: predialysis exercise, participating in various group workshops or following a personalised programme at home. Activities in daily life are also a way to get moving: walking the dog, gardening, going on foot to the store to buy bread or doing the housework etc.
It is important to remember that any increase in physical activity, even minimal, may be beneficial, so we must move whenever possible! Do not hesitate to talk about physical activity with your doctor!
Catherine Lasseur, France
References
- Phenotypes influencing low physical activity in maintenance dialysis. Panaye M, Kolko-Labadens A, Lasseur C, Paillasseur JL, Guillodo MP, Levannier M, Teta D, Fouque D. J Ren Nutr. 2015 Jan;25(1):31-9.
- Physical activity in dialysis population: how and why to assess and establish a program? Kolko Labadens A, Lasseur C, Labat T, Trolonge S, Chauveau P. Nephrol Ther. 2014 Jun;10(3):151-8.
- Physical exercise among participants in the Dialysis Outcomes and Practice Patterns Study (DOPPS): correlates and associated outcomes. Tentori F1, Elder SJ, Thumma J, Pisoni RL, Bommer J, Fissell RB, Fukuhara S, Jadoul M, Keen ML, Saran R, Ramirez SP, Robinson BM. Nephrol Dial Transplant. 2010 Sep;25(9):3050-62. doi: 10.1093/ndt/gfq138. Epub 2010 Apr 13.
- Barriers to exercise participation among dialysis patients. Delgado C1, Johansen KL. Nephrol Dial Transplant. 2012 Mar;27(3):1152-7. doi: 10.1093/ndt/gfr404. Epub 2011 Jul 26.
Potassium
It is common for patients undergoing haemodialysis to have elevated levels of potassium. Therefore, they should be advised to choose fruit and vegetables with a low or medium potassium level and to avoid rich sources of potassium.
Patients should also avoid chocolate, coffee, peanut butter, praline and salt substitutes as they are rich in Potassium chloride.
Some practical ways to limit potassium content in fruit and vegetables are:
- Peel fruit and vegetables that can be peeled, for example, potatoes, tomatoes, carrots, apples and pears.
- Cut fruit and vegetables into very small pieces before you consume them.
- Leave vegetables in plenty of fresh water for at least two hours before cooking them. Rinse them before cooking.
- Boil vegetables for 5 minutes in a big pot and then change the water and continue cooking for the rest of the time needed.
KalliopiAnna Poulia, Greece
Protein Intake for CKD Patients
Most recent studies show that eating too much protein is associated with a more rapid decline in kidney function. Reducing protein intake in the later stage of CKD delay the time dialysis start. This has been integrated into the recent KDOQI guidelines. At the early stage (1 to 3a, GFR 45 ml/min) a normal protein intake of no more than 0.8 g/kg/J is recommended. At a later stage, a decrease to 0.6 g/Kg/J or 0.4 supplemented with amino acids/ketonalogs demonstrated beneficial effects on renal function and quality of life. Energy intake should be maintained at a normal level. Regular dietitian advice helps you to progressively decline protein intake. Such a reduction may not be too complicated (or too restrictive) with the help of low or no-protein products.
Bread and cookies or pasta, low in protein, salt and phosphorus are available in Europe. Even if recent cohort studies suggest that a vegetable-based diet, such as the Mediterranean diet, has a beneficial effect (more fibre intake, less phosphate absorption, better lipid profile) there is actually no evidence to recommend a specific protein type plant vs animal.
Regular check-ups and advice from a dietitian help the patient to find a balance between the pleasure of eating and a protein-restricted diet.
Philippe Chauveau, France
Protein intake for hemodialysis patients
Protein needs are elevated for patients in haemodialysis due to the loss of amino acids during the treatment. Patients would therefore be advised to increase their daily protein intake. According to the most recent guidelines, patients are advised to consume a sufficient amount of protein to compensate for losses during haemodialysis. This amount is equal to 1.0-1.5g of protein per kg per day.
Food items rich in protein with a “high biological value”, such as meat, poultry, soya and egg whites are extremely important. Every 30g of meat or poultry provides 7g of protein to our body. Although fish and dairy products are sources of high biological value protein, they are also high in phosphate and should be chosen with caution according to dietitian/nutritional advice.
Food items that are sources of protein with a “low biological value”, such as legumes, grains and seeds should be limited as they are also good sources of phosphate and potassium. In case of constipation, however, whole wheat cereals could be added to the diet in order to help resolve the problem.
KalliopiAnna Poulia, Greece
Sodium
Sodium, together with potassium and chloride, is one of the three major electrolytes in the body. Sodium contributes to the regulation of blood pressure and volume, the transmission of impulses for nerve function and muscle contraction.
The relationship between salt intake and blood pressure was discovered about 4,000 years ago when Chinese emperor Huang Ti drew a connection between salt and a “hardened pulse”. Today, salt is the most suspected environmental factor that may influence blood pressure and atherogenesis. The World Health Organisation recommends a reduction to < 2g/day sodium (5g/day salt) in adults, which helps to prevent blood pressure-related cardiovascular events and strokes (1).
Public awareness about the potentially adverse role of high sodium chloride consumption was first raised by a study in Finland that showed high sodium intake predicted mortality, particularly in males and overweight individuals during a 17-year follow-up (2).
According to the meta-analysis by Feng J He et al, a modest reduction in salt intake for four or more weeks causes a significant fall in blood pressure in both hypertensive and normotensive individuals, irrespective of sex and ethnic group (3).
The exaggerated blood pressure response to dietary salt intake affects approximately 50% of hypertensive patients and 25% of normotensive adults (4).
The risk of salt sensitivity increases with age, the presence of obesity or diabetes and a decline in renal function. Guidelines from the KDIGO (in ‘Clinical Practice Guidelines for the Evaluation and Management of Chronic Kidney Disease’) recommend lowering salt intake to 90mmol (2g) per day of sodium (corresponding to 5g of sodium chloride) in adults unless contraindicated (5).
Salt restriction is not recommended in patients with salt-wasting nephropathies and those prone to hypotension and volume contraction. In the early stages of chronic kidney disease, increased salt intake contributes to the prevalence of hypertension and proteinuria. For the same amount of salt intake, patients with kidney disease show a higher hypertensive response than those with normal renal function (6).
Dietary salt excess may also attenuate the antihypertensive and antiproteinuric effects of antihypertensive drugs (7,8).
Although there is some evidence that salt ingestion could attenuate kidney damage independent of blood pressure, the data searching for the association between dietary sodium restriction and the progression of kidney disease and mortality is not supportive (9).
From a historical perspective, salt was primarily used to preserve food. In industrialised countries, most sodium intake comes from salt added during food processing. Convenience foods such as fast food, frozen dinners, packaged side dishes, sauces, snacks, ready-made soups, cheese and pastry may be high in sodium. Salt might have been added to processed food like meat, bread and cereals to retain moisture and enhance flavour. Restaurant meals and fast food may also contain high amounts of salt.
Tips to decrease sodium intake:
- Prepare meals from fresh food.
- Try to use fresh poultry, fish and meat rather than canned, smoked or processed products.
- Avoid fast foods, frozen dinners and canned foods.
- Use sodium-free seasonings to add flavour to your food instead of salt including herbs, spices, garlic, shallots, parsley, onion and lemon juice.
- Check the sodium content on food labels for sauces, snacks etc. A daily value of 20 per cent or more means the food item is high in sodium.
- Look for terms like sodium-free or salt-free, low, reduced, or no salt or sodium; or unsalted or lightly salted on labels.
- Beverages might contain added sodium, so check the ingredients.
- Baked food may include salt, therefore consume bread products low in sodium or without any added salt.
- Dietary salt or low-salt foods may contain salt substitutes rich in potassium so check for their potassium content.
- Rinsing with water will decrease the sodium, potassium and phosphorus in canned food, beans, meats and fish; so rinse with water.
Siren Sezer, Turkey
Sodium and fluid intake in dialysis patients
Sodium accumulation is one of the consequences of renal failure, resulting in increased water intake, an increase in the extracellular volume and a rise in blood pressure (10). Strict volume control is associated with improved control of hypertension and prolonged survival in those on haemodialysis (11,12).
The ability of patients with kidney disease to detect or taste salt in food is often impaired (13). This may contribute to high levels of sodium in the body due to an increase in dietary consumption.
The kidney patient on a high sodium diet might complain about thirst, oedema and shortness of breath. Reducing dietary sodium intake will help to control blood pressure and fluid intake. In these patients, effective management of hypertension requires normalisation of sodium balance and volume excess through reaching the ideal dry weight (14,15).
Sodium intake in renal transplant patients
Reducing sodium intake is also recommended for patients with kidney transplants. In hypertensive kidney transplant patients, low sodium intake combined with antihypertensive therapy results in significantly decreased blood pressure versus those on therapy without sodium restriction (16).
The issue of high salt intake in chronic kidney disease patients resembles that of blood glucose control in diabetics. Gaining a self-management approach and autonomy in dietary habits should be an absolute priority in patients’ lives.
Remember: one teaspoon of salt has about 2,300mg of sodium, which is the recommended amount for the entire day!
Sugars and Carbohydrates
Polysaccharides usually contain from ten up to several thousand monosaccharides arranged in chains. The main types of polysaccharides are: Starch, cellulose, pectin, gums and fibre.
Starch – is probably the most common of the polysaccharides and it is made up of long chains of glucose. Starch is made by plants during photosynthesis. It is present in cereal grains (wheat, oats, rye, barley, buckwheat, rice, etc.), potatoes and legumes.
Cellulose – is another long chain polysaccharide made from many glucose building blocks. Cellulose is also called dietary fibre. We often talk about cellulose as dietary fibre or what we used to call “roughage” as the human body is unable to break it down during digestion.
Pectin – The word ‘pectin’ comes from the Greek word pektos, which means firm and hard. Pectin is present in virtually all plants where it contributes to the cell structure. The term pectin covers a number of polymers that vary according to their molecular weight, chemical configuration and content of neutral sugars. Pectin gives fruit its structure and firmness. Fruits high in pectin include apples and most citrus fruits.
Gums – are used primarily as thickeners in food. Some seaweeds are also excellent sources of gums and are commonly called carrageenan and alginates. They are often used as a vegetable substitute for gelatin.
Glycogen – is the stored form of glucose in the human body. The body stores glycogen in the liver, muscles and brain.
Vitamins
Vitamins do not contain any calories. They serve the great functions of life (Vitamin A helps our sight, Vitamin D the bones and the B vitamins help the nervous system and hematocrit etc …).
We classify them into two groups:
- Fat-soluble vitamins that are soluble in fats: Vitamins A, D, E and K.
- Water-soluble vitamins that are soluble in water: Vitamins C, B1, B3 or PP, B5 or Pantothenic acid, B6, B8 or Biotin, B9 or Folic acid and B12.
Philippe Chauveau, France