Sugars and Carbohydrates
Was ist ein Kohlenhydrat?
Polysaccharides usually contain from ten up to several thousand monosaccharides arranged in chains. The main types of polysaccharides are: Starch, cellulose, pectin, gums and fibre.
Starch – is probably the most common of the polysaccharides and it is made up of long chains of glucose. Starch is made by plants during photosynthesis. It is present in cereal grains (wheat, oats, rye, barley, buckwheat, rice, etc.), potatoes and legumes.
Cellulose – is another long chain polysaccharide made from many glucose building blocks. Cellulose is also called dietary fibre. We often talk about cellulose as dietary fibre or what we used to call “roughage” as the human body is unable to break it down during digestion.
Pectin – The word ‘pectin’ comes from the Greek word pektos, which means firm and hard. Pectin is present in virtually all plants where it contributes to the cell structure. The term pectin covers a number of polymers that vary according to their molecular weight, chemical configuration and content of neutral sugars. Pectin gives fruit its structure and firmness. Fruits high in pectin include apples and most citrus fruits.
Gums – are used primarily as thickeners in food. Some seaweeds are also excellent sources of gums and are commonly called carrageenan and alginates. They are often used as a vegetable substitute for gelatin.
Glycogen – is the stored form of glucose in the human body. The body stores glycogen in the liver, muscles and brain.
Simple Carbohydrates examples:
- Monosaccharides or simple sugars (1 sugar unit)
Fructose
Galactose
Glucose
Mannose
Tagatose
Xylose
- Disaccharides (2 sugar units)
Isomaltose
Isomaltulose
Lactose
Maltose
Sucrose
Trehalose
Trehalulose
- Dietary fibre
Erythritol
Glycerol
Hydrogenated starch hydrolysates
Isomalt
Lactitol
Maltitol
Mannitol
Sorbitol
Xylitol
Complex Carbohydrates examples:
- Oligosaccharides (3-10 sugar units)
Fructooligosaccharides (FOS)
Galactooligosaccharides (GOS)
Human milk oligosaccharides (HMO)
Isomalto-oligosaccharides (IMO)
Maltotriose
Mannan oligosaccharides (MOS)
Raffinose, stachyose and verbascose
- Polysaccharides (-10 sugar units)
Chondroitin sulfate
Dextrins
Glycosaminoglycans
Maltodextrins
Starch
- Dietary fibre
Soluble fibre:acacia (arabic) gum), agar-agar, algin, arabynoxylan, beta-glucan, carrageenan, carob (locust bean) gum, fenugreek gum, galactomannans, gellan gum, glucomannan (konjac gum), guar gum, hemicellulose, inulin, karaya gum, pectin, polydextrose, psyllium husk mucilage, resistant starches, tara gum, tragacanth gum, xanthan gum the oligosaccharides listed above, with the exception of maltotriose
Insoluble fibre: cellulose, chitin and chitosan
How much sugar do we need?
All carbohydrates are broken down to glucose during digestion. This glucose molecule undergoes a biochemical pathway to produce the energy molecule ATP (adenosine triphosphate).
The recommended limit for the daily dose of sugar for improved health is around 11 grams, or roughly no more than 5% of daily calorie intake. According to the World Health Organization (WHO), this number should never exceed 25 grams (4). A sugar-heavy diet is linked to increased risk of heart disease, diabetes, poor dental health, high blood pressure, high cholesterol and obesity (5).
The European Food Safety Authority defines sugar in food as “the total sugar”, including both endogenous (sugars naturally present in foods such as fruit, vegetables, cereals and lactose in milk products) and added sugars. The term ‘added sugars’ refers to sucrose, fructose, glucose, starch hydrolysates (glucose syrup, high-fructose syrup, isoglucose) and other isolated sugar preparations used as such, or added during food preparation and manufacturing (6).
What are the best types of carbohydrates?
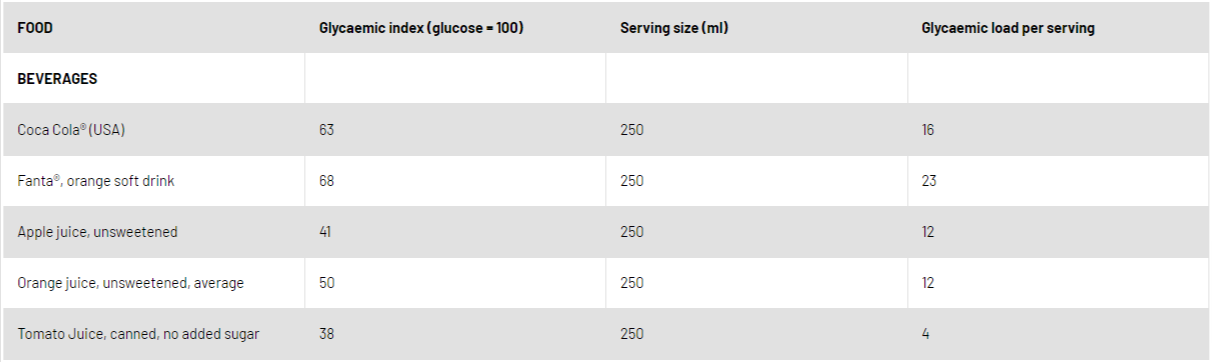
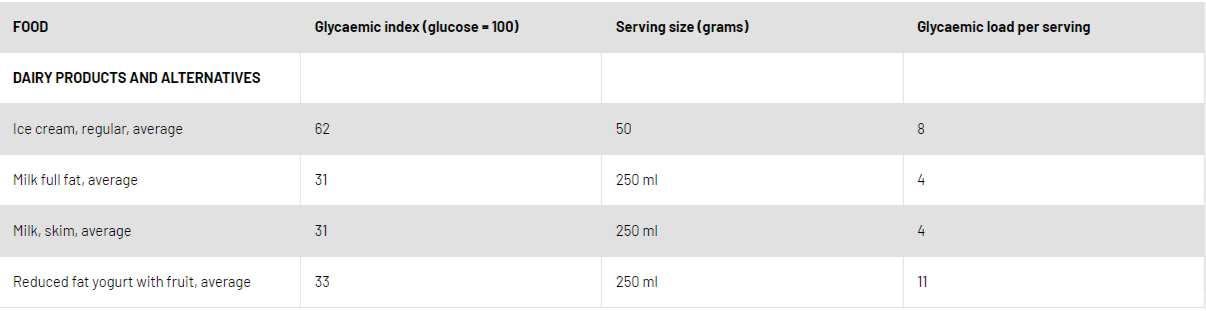
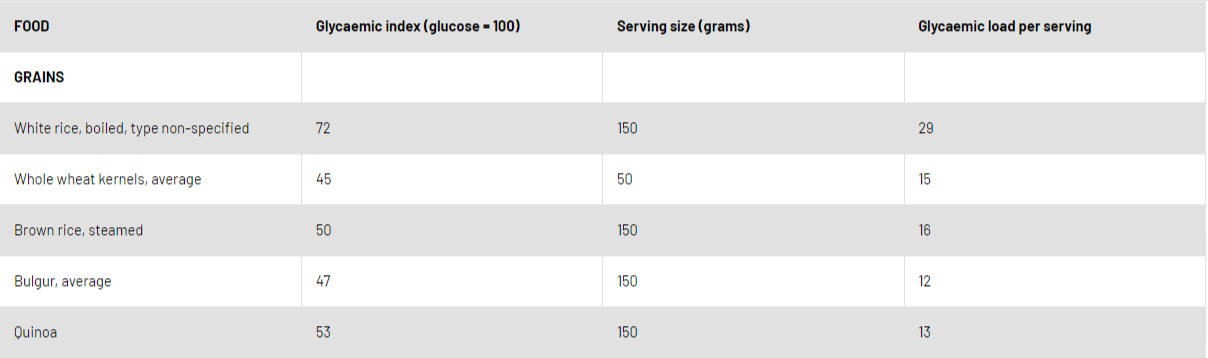
The plasma concentration of insulin increases immediately after the ingestion of glucose in the form of sugars or digestible starch. The glycaemic indicates how rapidly a carbohydrate is digested and released as glucose (sugar) into the blood stream. Glycaemic load is a ranking system for carbohydrate-rich food that measures the amount of carbohydrates in a serving of food and is determined by multiplying the grams of a carbohydrate in a serving by the glycaemic index, then dividing by 100. A glycaemic load of 10 or below is considered low; 20 or above is considered high. The glycaemic index and glycaemic load values of common food are listed in table 2 (9).
Simple carbohydrates are so small and their glycaemic index is high. When the diet consists of simple sugars and refined carbohydrates (which the body breaks down rapidly), elevations in blood triglyceride levels, bad cholesterol, and development of insulin resistance can be noticed. Prospective cohort studies indicate that diets with a higher glycaemic index or glycaemic load are associated with a greater risk of type 2 diabetes mellitus (7).
Simple carbohydrates are often softer in texture – white bread, white rice and baked goods. Soda, candy and other sweeteners like table sugar and honey are also simple carbohydrates. These easily digested carbohydrates are rapidly absorbed, causing a spike in blood sugar levels and a quick boost in energy. Refined flours have been stripped of some of their natural, high fibre content including bran, germ or endosperm. As a result of this processing, they are digested faster and more easily and deliver fewer amounts of healthy nutrients. Fruit, vegetables and dairy products are also technically made of simple carbohydrates, but because of the fibre, protein and other nutrients, they act more like complex carbohydrates in the body and should be consumed daily.
Complex carbohydrates are bigger and digested and absorbed slowly. Their glycaemic index is low, thus causing low rate insulin release, which may reduce triglycerides. Other benefits of consuming complex carbohydrates are enhanced satiety, increased fibre intake and better blood sugar control. Complex carbohydrates are found in legumes, whole grains, vegetables and fruit. Whole grains include whole wheat, whole wheat flour, wheat flakes, bulgar wheat, whole and rolled oats, oatmeal, oat flakes, brown rice, whole rye, rye flour and whole barley.
Dietary fibre has been defined as non-starch polysaccharide, comprising cellulose and non-cellulose polysaccharides (e.g. pectins, glucans, arabinogalactans, arabinoxylans, gums and mucilages).
According to their glycaemic index, foods can be divided into three groups (8):
Low Glycaemic Index Foods (55 or less):whole wheat or pumpernickel bread, oatmeal oat bran, muesli, pasta, converted rice, barley, bulgar, sweet potato, corn, yam, lima/butter beans, peas, legumes and lentils, most fruits, non-starchy vegetables and carrots.
Medium Glycaemic Index (56-69): Whole wheat, rye and pita bread, quick oats, brown, wild or basmati rice and couscous.
High Glycaemic Index (70 or more): White bread or bagel, corn flakes, puffed rice, bran flakes, instant oatmeal, shortgrain white rice, rice pasta, macaroni and cheese from mix, russet potato, pumpkin, pretzels, rice cakes, popcorn, saltine crackers, melons and pineapple.
Choosing whole fruit instead of juice, a whole grain side dish instead of crackers and fresh vegetables instead of potato chips will ensure getting complex carbohydrates.
Give more attention to fructose:
While glucose and fatty acids are used as key energy substrates, fructose cannot be used and has to be pre-processed in splanchnic organs. The unregulation of the phosphorilating enzyme in this process leads to lower ATP pools, moreover, to stimulate hepatic nucleotide turnover and uric acid production. Clinical evidence has also shown that hyperuricaemia and fructose consumption may also increase blood pressure in adults (10).
The consumption of sugar has increased in the western world and high fructose corn syrup in sugar-sweetened soda/beverages has contributed to this increase (11). Sugar is also taken with candy and baked items, but its consumption can be difficult to control because the food industry often adds it where consumers might not think to check. Fructose consumed may promote visceral adiposity, increased hepatic de novo lipogenesis and hypertension together with hyperuricaemia (1). In animal models, fructose promotes sodium reabsorption in the kidney, providing new insight into the possibility that fructose has a role in the salt-sensitivity of blood pressure (12).
Epidemiologic data has quantified the relationship between sugar-sweetened beverage consumption obesity, type 2 diabetes and cardiovascular disease risk (13). Sugar-sweetened beverages contribute to weight gain in part by additional intake of liquid calories, high dietary glycaemic load leading to inflammation, impaired β-cell function and insulin resistance. A cross-sectional analysis of over 9000 participants in the National Health and Nutrition Examination Survey (NHANES) 1994-2004 reported a significant association between early kidney disease (based on microalbuminuria) and consumption of ≥2 sugar soft drinks per day (14).
What should a kidney patient eat?
Healthy dietary patterns are associated with lower mortality in patients with kidney disease. In the meta-analysis including 15,285 participants with kidney disease who consumed higher quantities of fruit and vegetables, fish, legumes, cereals, whole grains, fibre and lower amounts of red meat, salt and refined sugars had increased survival rates (15).
NKF-KDOQI guidelines and the International Society of Renal Nutrition and Metabolism recommend a total energy intake of 30–35kcal/kg BW/day, which should be tailored to physical activity levels [16, 17]. In elderly patients who are sedentary, energy intake of 30 kcal/kg BW/day may be sufficient. These recommendations apply to all non-dialysis and dialysis dependent CKD patients irrespective of their aetiology of kidney disease (i.e. diabetic and non-diabetic kidney disease).
Given that ~45–60% of energy intake is obtained from carbohydrate sources, careful consideration should be made with respect to the source of dietary carbohydrates. For example, carbohydrates from sugars should be restricted to less than 10% of energy intake, and higher glycemic index foods should be substituted with low glycaemic index foods such as whole grains, fibre, fresh fruit, and vegetables (18,19). Intake of complex carbohydrates with high fibre has been found to reduce dietary phosphorus and protein as well as urea and creatinine generation(20).
The glycaemic index and glycaemic load of common food (9).
Siren Sezer, Turkey

Ernährungstabellen
Referenzen
- Kohlenhydrate als Energiequelle. Jéquier E. Am J Clin Nutr.1994 März;59(3 Suppl):682S-685S.
- http://www.fao.org/docrep/008/y4705e/y4705e09.htm
- SACN. Kohlenhydrate und Gesundheit. 2015. Verfügbar unter https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf
- WHO. Zuckeraufnahme für Erwachsene und Kinder-Leitlinie. 2015. Verfügbar unter: http://www.who.int/nutrition/publications/guidelines/sugars_intake/en/. Abgerufen im Apr 2016.
- Zusammenhang zwischen Zuckerverbrauch und Risikofaktoren für chronische Krankheiten: Aktuelles Verständnis.James M. Rippe1,2,*und Theodore J. Angelopoulos Nutrients. 2016 Nov; 8(11): 697.
- https://www.efsa.europa.eu/en/press/news/170323-0
- Glykämischer Index, glykämische Last und Risiko für Typ-2-Diabetes: Ergebnisse aus 3 großen US-Kohorten und eine aktualisierte Metaanalyse. Shilpa N Bhupathiraju, Deirdre K Tobias, Vasanti S Malik, An Pan, Adela Hruby, JoAnn E Manson, Walter C Willett, Frank B Hu Am J Clin Nutr. 2014 Jul; 100(1): 218–232
- Kanadische Diabetes-Gesellschaft (CDA). Das Werkzeug Glykämischer Index. Online verfügbar: http://www.diabetes.ca/for-professionals/resources/nutrition/glycemic-index/ (abgerufen am 14. März 2010).
- Internationale Tabelle von glykämischen Indexen und glykämischen Ladewerten: 2002. Kaye Foster-Powell, Susanna HA Holt, und Janette C Brand-Miller. Am J Clin Nutr 2002;76:5–56.
- Gicht. Richette P,Bardin T. Lancet 2010 Jan 23;375 (9711):318-28
- Fructose und metabolische Krankheiten: neue Erkenntnisse, neue Fragen. Tappy L, Lê KA, Tran C, Paquot N.Nutrition.2010 Nov-Dec;26(11-12):1044-9.
- Eine moderate (20%) fruktoseangereicherte Diät stimuliert bluthochdruckempfindlichen Bluthochdruck mit erhöhter Salzretention und verminderter Nierenstickoxidproduktion. Gordish KL, Kassem KM, Ortiz PA, Beierwaltes WH. Physiol Rep. 2017 Apr;5(7): e13162.
- Zuckerhaltige Getränke und Risiken für kardio-metabolische Erkrankungen.Bjorn Richelsen. Current Opinion in Clinical Nutrition and Metabolic Care 2013: 16(4):478-484
- Shoham DA, Duraza-Arvizu R, Kramer H, Luke A, Vup-puturi S, Kshirsagar A, Cooper RS. Zuckergetränke und Albuminurie: Ergebnisse aus der National Health and Nutrition Examination Survey, 1999-2004. PLoS ONE 3:e3431,2008
- Gesunde Ernährungsmuster und Sterblichkeits- und ESRD-Risiko bei CKD: Eine Metaanalyse von Kohortenstudien. Jaimon T Kelly, Suetonia C Palmer, Shu Ning Wai, Marinella Ruospo, Juan-Jesus Carrero, Katrina L Champbell, Giovanni F M Strippoli. Clin J Am Soc Nephrol 2017:12:272-279
- Kopple, J.D. National Kidney Foundation K/DOQI klinische Praxisrichtlinien für die Ernährung bei chronischer Niereninsuffizienz. Am. J. Kidney Dis. 2001, 37, S66–S70
- Ikizler, T.A.; Cano, N.J.; Franch, H.; Fouque, D.; Himmelfarb, J.; Kalantar-Zadeh, K.; Kuhlmann, M.K.; Stenvinkel, P.; TerWee, P.; Teta, D.; et al. Prävention und Behandlung von Proteinenergiemangel bei Patienten mit chronischer Nierenerkrankung: Eine Konsenserklärung der International Society of Renal Nutrition and Metabolism. Kidney Int. 2013, 84, 1096–1107.
- Ley, S.H.; Hamdy, O.; Mohan, V.; Hu, F.B. Prävention und Management von Typ-2-Diabetes: Nahrungskomponenten und ernährungsstrategien. Lancet 2014, 383, 1999–2007.
- KDOQI. KDOQI klinische Praxisleitlinien und klinische Praxishinweise für Diabetes und chronische Nierenerkrankung. Am. J. Kidney 2007, 49, S12–154.
- Chiavaroli L, Mirrahimi A, Sievenpiper JL, Jenkins DJ, Darling PB. Effekte von diätetischer Faser auf chronische Nierenerkrankung: Eine systematische Überprüfung und Metaanalyse von kontrollierten Fütterungsstudien.Eur J Clin Nutr2015;69:761-768